Everyday pathology
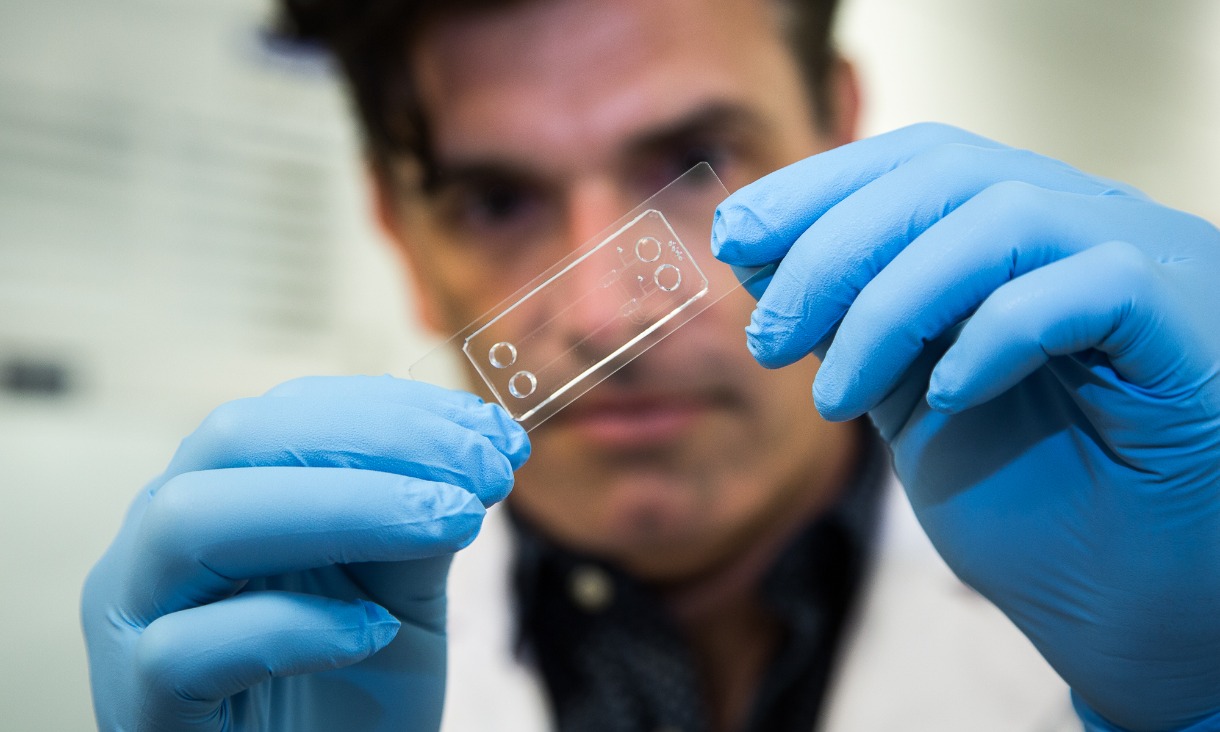
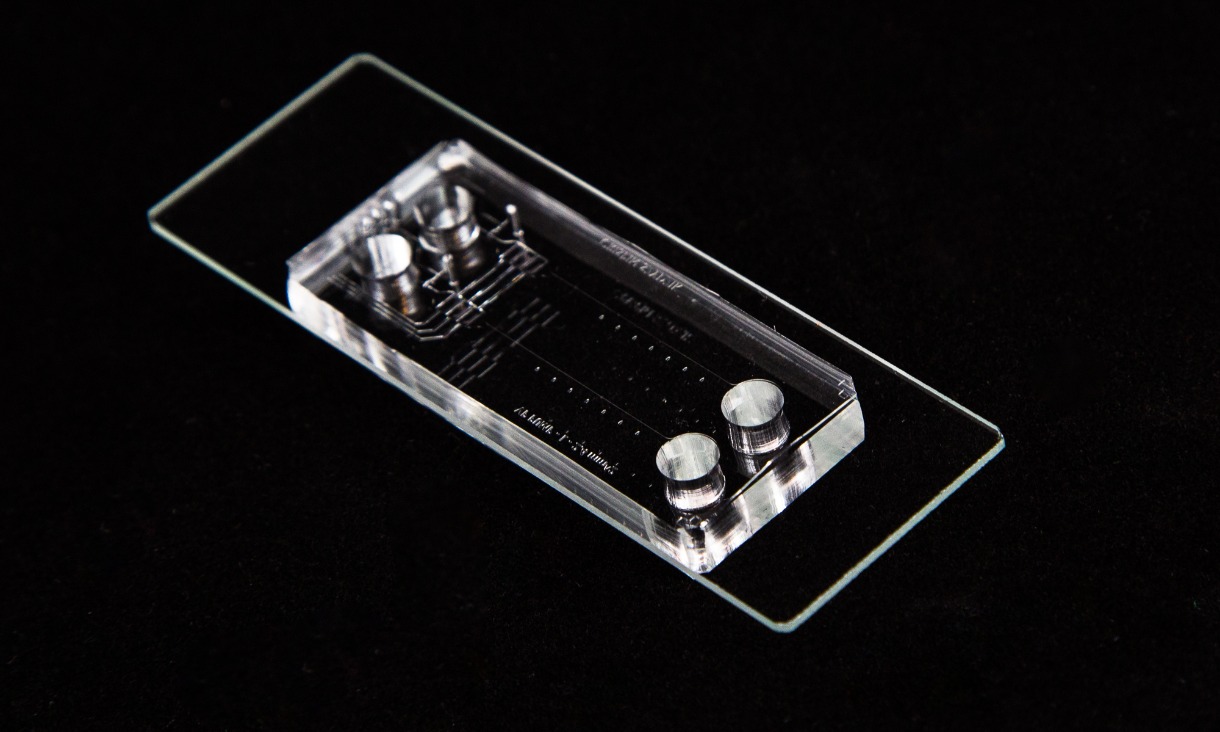
The microfluidic chips being developed by the team contain tiny channels, pumps, valves and processors, enabling precise and flexible manipulation of fluids.
The chips are fast, portable and able to handle vast quantities of tiny processing elements. Importantly, they are also cost-effective to produce and can be easily mass manufactured.
When combined with a highly sensitive photonic sensor, for biochemical analysis, the technology effectively becomes a miniature laboratory – a lab-on-a-chip – but one that needs no specialist training to use.
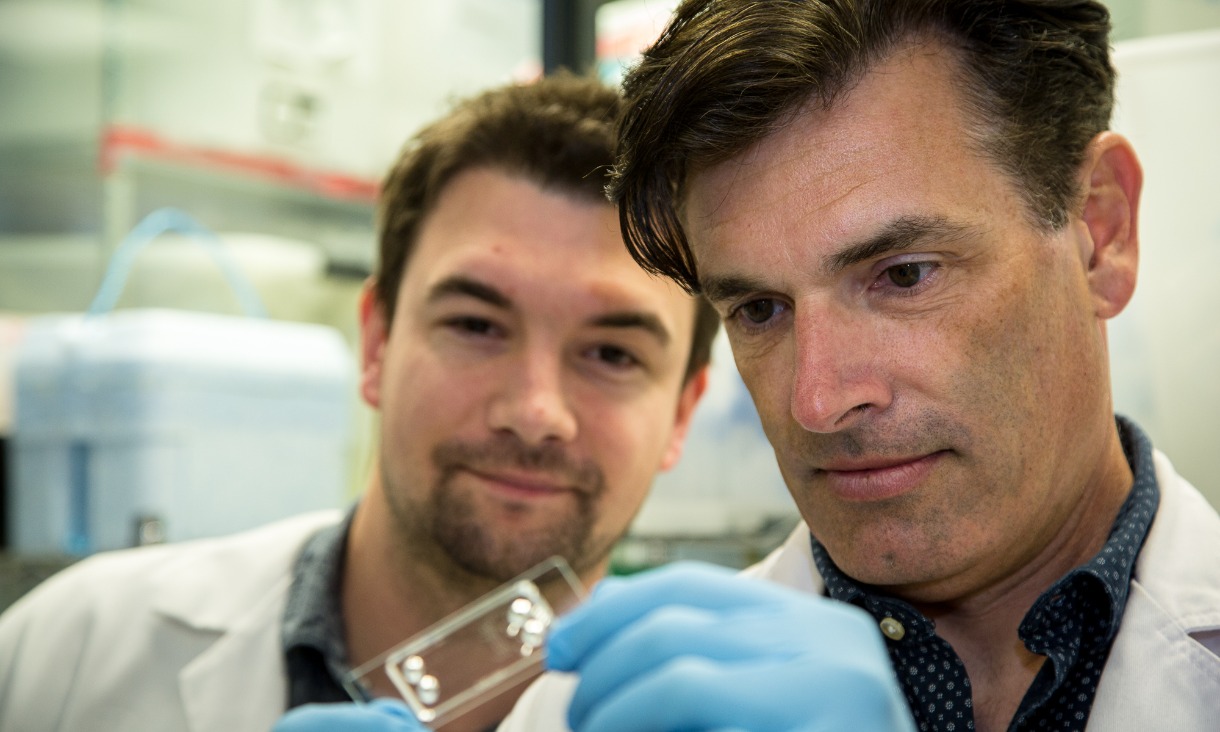
“Because whole blood is so complex, most blood diagnostic tests tend to involve some form of processing, such as spinning out red blood cells,” Nesbitt says.
“Pathology lab tests are technically demanding and expensive. You need a highly-trained medical scientist that is experienced in blood separation techniques and analysis to ensure consistency of results.
“Our ultimate aim is to make lab-on-a-chip devices that an unskilled operator can use, that can either do the processing inside the device or work with blood taken straight from patients.
“This is particularly important for regional areas, where emergency clinics with no in-house pathology services can face long delays in waiting for results.”
Precision and reliability
Nesbitt and the team at the MNRF develop micro devices that can be used for three key aspects of blood: bleeding, clotting and detecting biomarkers.
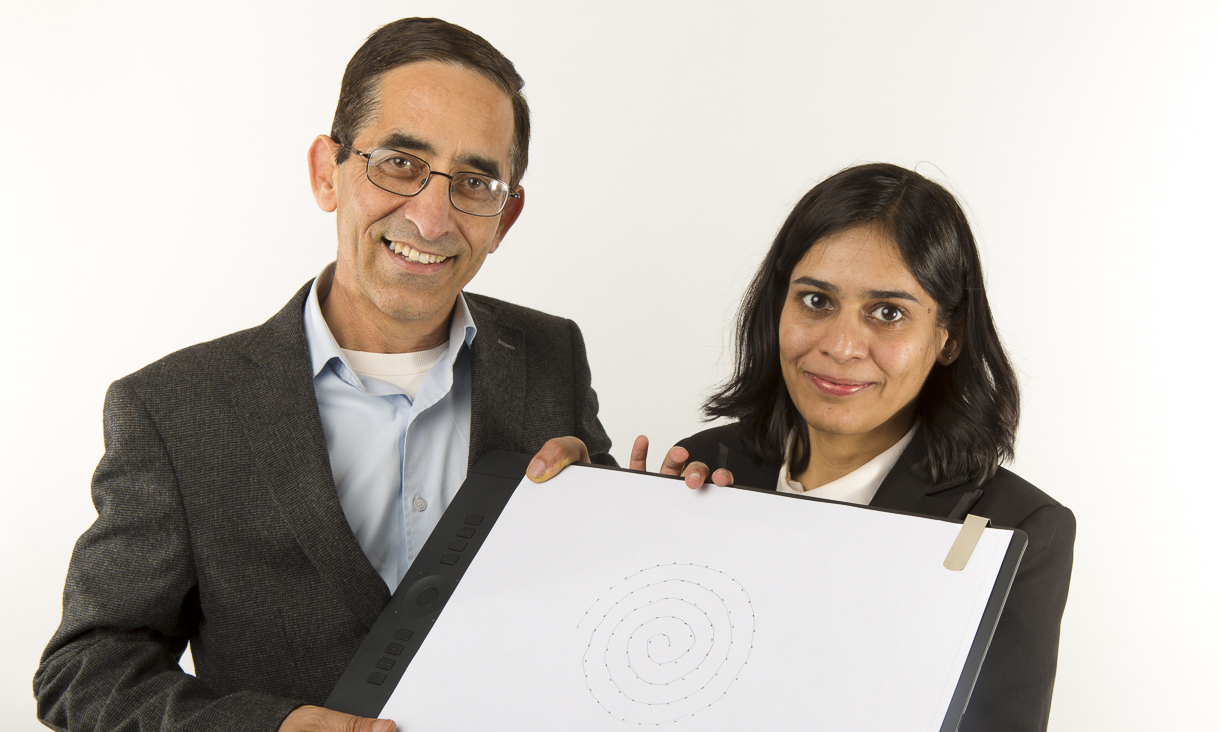
The researchers have worked on the diagnosis and monitoring of the most common genetic bleeding disorder, Von Willebrand disease (VWD).
Current testing of VWD involves laboratory-based assays along with clinical assessment. In addition certain forms of the disease can be difficult to diagnose.
The RMIT team’s proof-of-concept trial showed their tailored micro device could detect the particular forms of the disease that are most difficult to spot with standard tests.
“Blood from healthy people behaves differently to the blood of someone with VWD,” Nesbitt explains.
“If the blood is from a healthy person, the platelets clump together to form a mini thrombus.
“They don’t clump in someone with VWD and that’s what we can measure with great precision - exactly how much the platelets cluster together.”


.jpg)
