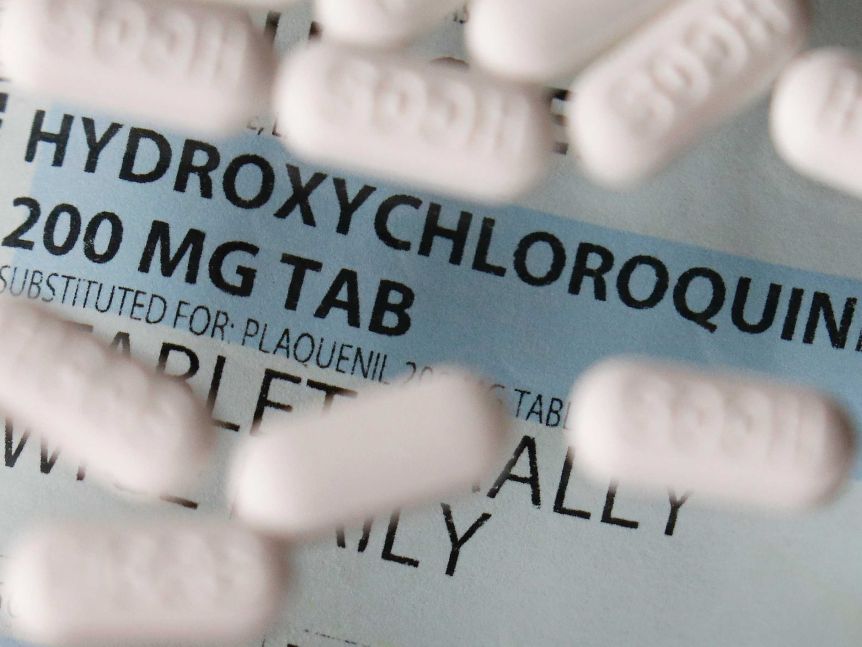
On April 1, Mr Hunt told A Current Affair he had just spoken to "an international supplier" and was "confident that we will have a significant supply of hydroxychloroquine, which will be available if doctors wish to use them with patients who are in hospital. Those are the terms".
On April 2, the Secretary of the Department of Health created an exemption under the Therapeutic Goods Act 1989 to allow the Government to stockpile hydroxychloroquine.
However, the department told Fact Check this was "not blanket approval or endorsement for the use of the drug for COVID-19".
Is it being used widely?
Professor Dore said that for a drug to dent the mortality curve, it would need to be both very effective and widely used among patients.
But while Mr Palmer said hydroxychloroquine had kept a lid on Australia's COVID-19 deaths, Fact Check found little evidence of widespread use.
The federal health department said it did not collect information on which drugs patients were receiving.
In a written statement, NSW Health said it "understands a small number of COVID-19 patients in NSW has received hydroxychloroquine prescribed by individual medical practitioners".
Fact Check approached the Victorian Health Minister but did not receive a response.
Professor Cheng said his hospital, one of Melbourne's largest, did not routinely prescribe the drug to COVID-19 patients and he "would be pretty surprised if it was [given to] more than a handful of patients".
Some national data on hydroxychloroquine use is available through a hospital surveillance study called SPRINT-SARI, Professor Cheng said, but this only covered patients in intensive care.
By April 26, intensive care patients accounted for fewer than 20 per cent of COVID-19 hospitalisations.
Does the drug work?
Mr Palmer's claim that hydroxychloroquine helped reduce mortality assumes the drug is effective in treating COVID-19.
But while his Palmer Foundation website refers to a number of studies on the topic, the evidence available when he made his claim was not encouraging.
In a report published on April 14, experts from Oxford University's Centre for Evidence Based Medicine critiqued five clinical trials and found none of them "support the view that hydroxychloroquine is effective in the management of even mild COVID-19 disease".
The Doherty Institute's Steven Tong, who is leading an Australian clinical trial for COVID-19 treatments, also published a detailed summary of six treatment studies available before Mr Palmer's April 23 statement.
Released on May 6, the critique covered two more studies published before Mr Palmer's April 29 interview.
"The existing data do not provide sufficient evidence to conclude that there is a clear benefit, lack of benefit or harm," Associate Professor Tong wrote.
"The observational datasets are prone to bias. The [randomised control trials] are too small and have not reported on clinically relevant outcomes."
Professor Bennett told Fact Check that without control trials where people in similar risk categories were prescribed or not prescribed the drug, "you can claim whatever you like, but there are too many moving pieces".
Analysing the largest of the studies shared on Mr Palmer's website — a case series of 1,061 patients with no control group — she said 95 per cent of patients had mild or no symptoms at the outset, while the more serious cases represented "numbers too small to compare with other COVID patient treatment studies".
Professor Dore told Fact Check:
"We're still waiting for the large randomised control trial evidence one way or the other. So I don't think we can say that it has efficacy, but we can't rule it out either."
Mr Palmer, too, has acknowledged the need to wait for the trial results, telling the Sunrise program: "If we have a successful trial and we don't have the drug, what good is it? ... I wanted to make sure that if the Government wants to approve it, if it wants to allow it out, we'd have the material."
Since then, two large-scale observational studies in New York City and New York state have been published, each with roughly 1,400 COVID-19 hospital patients.
Neither found hydroxychloroquine significantly reduced the risk of death, and while both studies lacked control groups, experts said they were robust analyses.
Principal researcher: David Campbell, with Caitlin Cassidy.