
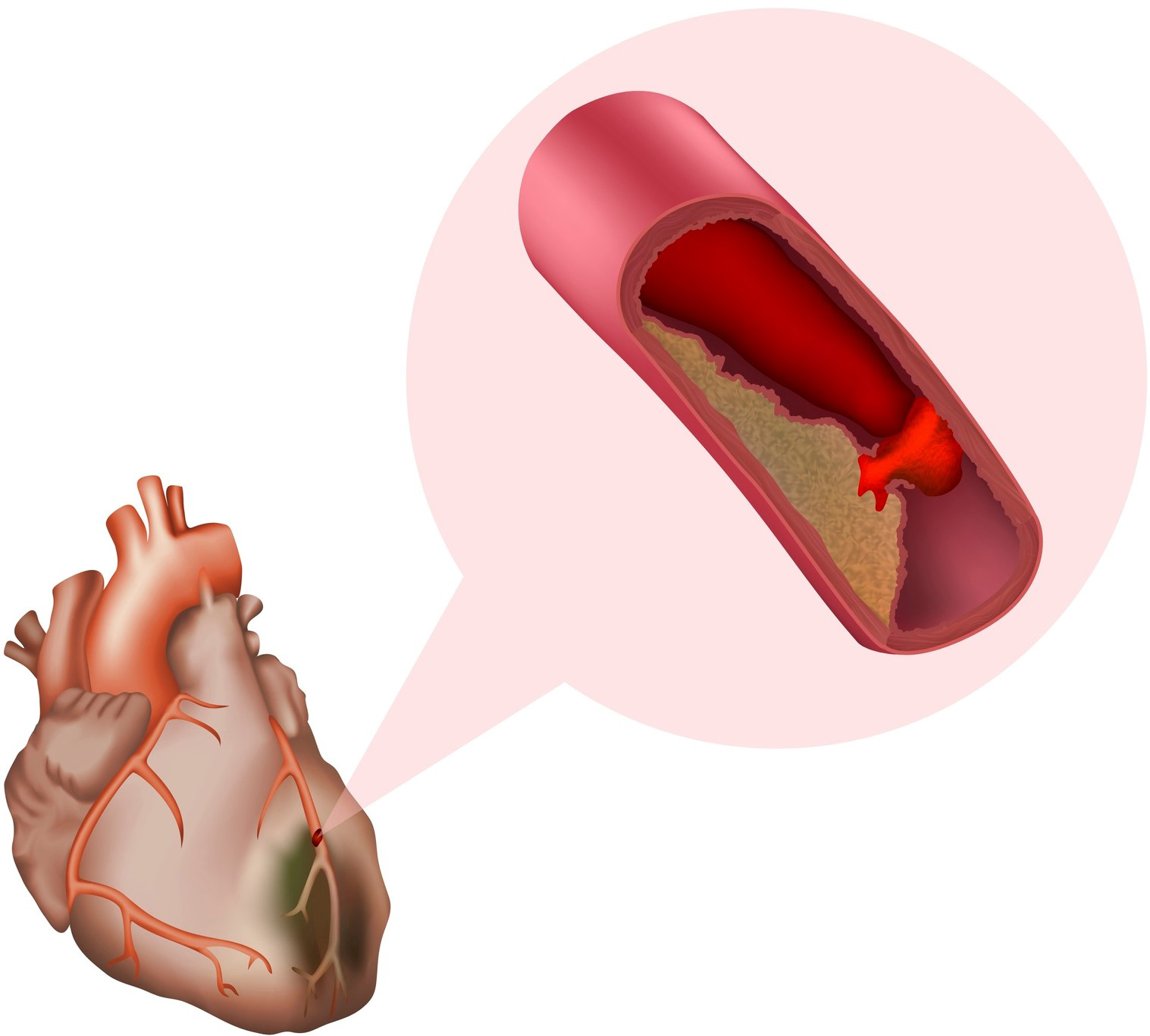
The leading cause of deadly heart attacks is the build-up of fatty deposits called ‘plaques’ in the walls of arteries. If an unstable plaque ruptures, it can completely block smaller blood vessels downstream stopping the heart muscle from getting the oxygen it needs. An angiogram is currently the best way to measure plaque build-up by determining its presence and degree of narrowing – but this test lacks the ability to accurately distinguish between a stable and an unstable plaque.
Currently, when a plaque is found, treatment will only be administered if the artery is blocked by more than 70 per cent – yet evidence suggests unstable plaques can cause heart attacks well below this threshold. More accurate detection of unstable plaques is therefore critical to saving lives.
Professor Karlheinz Peter and Matthew Hoskins from the Baker Institute, along with Professor Paul Stoddart from Swinburne University founded Nirtek to create a device that can find unstable plaques. The device uses laser imaging to immediately insert a stent to stabilise it. Nirtek engaged with us to establish a low-cost optic fibre based beam forming system that is compact and can be ramped up to large-scale manufacture.
After several iterations, the team created a photonic device that allows the detection of small unstable regions within the coronary arteries of the heart. The device can be inserted through a catheter to illuminate plaques within the arteries with laser light. When infra-red light is shone on unstable plaques, they auto-fluoresce, alerting the cardiologist to the need for treatment such as a stent or targeted medication to stabilise the plaque.
This is the first technology capable of detecting unstable plaques before they rupture and cause blockage, ultimately detecting heart attacks before they happen.
The InPAC team were valuable partners in the design and prototyping process, and we look forward to further engagement with this highly skilled team.
Matthew Hoskin
Nirtek CEO
April 2020: First team meeting with Nirtek via the medical device partnering program
Aug 2020: Began literature review, simulation, and design of NIRAF guidewire
Oct 2020: Started fabrication of first prototypes
Dec 2020: Prototyped the first component aimed to detect blockages
Jan 2021: Nirtek are looking for investors
Feb 2021: Nirtek announces the NIRAF guidewire device
Read more about the partnership on the Baker website.


RMIT University acknowledges the people of the Woi wurrung and Boon wurrung language groups of the eastern Kulin Nation on whose unceded lands we conduct the business of the University. RMIT University respectfully acknowledges their Ancestors and Elders, past and present. RMIT also acknowledges the Traditional Custodians and their Ancestors of the lands and waters across Australia where we conduct our business - Artwork 'Sentient' by Hollie Johnson, Gunaikurnai and Monero Ngarigo.
Learn more about our commitment to Indigenous cultures